HOW CAN PEOPLE WITH DEMENTIA EAT AND DRINK WELL? by Catriona Lawson, ANutr
Posted on
Dementia is a chronic and progressive condition and has a range of behavioural and cognitive symptoms. These include reduced communication skills and reasoning, memory loss, personality change and a reduced ability to undertake daily activities.1
There are over 200 subtypes of dementia. The most common subtypes in the UK include:
- Alzheimer’s disease (AD) (50-75%)
- Vascular dementia (up to 20%)
- Dementia with Lewy bodies (10-15%)
- Frontotemporal dementia (2%)2
1. Eating and drinking difficulties can create poor health and stress in those with dementia.
People with dementia may be unable to express when they are hungry or thirsty due to their decreased communication skills. They may communicate their needs by spitting food out or refusing to eat. Low mood may cause poor concentration and a lack of interest in food. It may be difficult for people with dementia to sit down for a meal due to agitation or anxiety.3
2. People with dementia may forget to eat and drink
They may also not remember that they have already eaten and had something to drink too. This may result in meals being skipped or even in overeating.4 There can be a lack of coordination, an inability to feed oneself, increased difficulties with chewing and swallowing and decreased thirst, in the later stages of dementia.3
3. Dysphagia can result in 13-57% of people living with different types of dementia
People may keep food in their mouth, be unable to form a bolus and have difficulties in the initiation of swallowing. Choking, coughing or wet voice when eating and drinking are other signs that a person has dysphagia.4

SO, HOW CAN PEOPLE WITH DEMENTIA EAT AND DRINK WELL?
Eating is an action that people with dementia can continue with and it helps keep their independence for as long as possible.3 It is important for people with dementia to eat well as weight loss/decrease in body mass can cause a more rapid progression of dementia. It can also increase the risk of dementia complications such as pressure sores, falls, fractures and infections.5,6
Food first
A food-first approach can address poor dietary intake and weight loss by increasing nutrient intake through a variety of ways. Providing a food-first approach to those with dementia can improve their nutrition by using food fortification to maximise nutrient density.4 High-energy snacks, nutritious drinks and eating little and often are strategies that can help improve energy and nutrient intake. NICE clinical guideline (CG32) stresses that the overall nutrient intake of oral nutrition support offered should include a balanced mixture of nutrients and not just calories.7
Fluid intake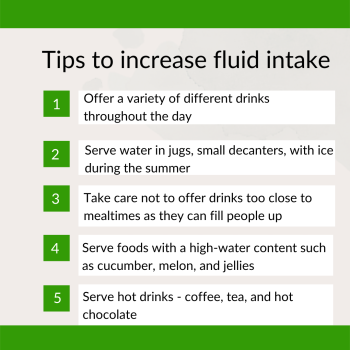
It is important to maintain fluid intake in people with dementia to prevent dehydration. Dehydration can increase risk of other health conditions such as constipation, poor oral health, and incontinence.3
Mouth care
Good mouth care is important for people with dementia on a pureed or thickened food diet and for those who prefer sweet foods and those who consume snacks frequently.8 People with dementia should be encouraged to drink milk. It is rich in calcium and phosphorus and a good source of protein. Good mouth care can be achieved by brushing teeth with fluoride toothpaste twice daily, cleaning dentures twice daily and having regular dental checks. This helps to maintain the ability to eat, improve taste and avoid gum or mouth infections.5
MALNUTRITION

Eating and drinking should be enjoyed as much as possible through the progression of the disease. However, people with dementia can develop problems with eating and drinking, such as dysphagia, which increases the risk of malnutrition. Malnutrition can contribute to the progression of dementia and can increase the risk of dementia complications. Balancing a food-first approach with adequate fluid intake to prevent dehydration, is essential to prevent undernutrition.
Eating and drinking are activities that people with dementia can enjoy for as long as possible. Putting strategies in place to support a healthy balanced diet and consideration of the eating environment to make it a positive experience at mealtimes, mitigates some of the challenges and helps maintain a person's independence and dignity.
Catriona Lawson, ANutr
Freelance Nutritionist
Catriona worked in care home as a nutritionist for the elderly with dementia.
She is currently a freelance nutritionist and member of the
public involvement network with the Advanced Care
Research Centre at the University of Edinburgh.
Twitter@CatrionaLawson1
www.catrionanutritionblog.com
References
- National Institute for Health and Care Excellence. Dementia: assessment, management and support for people living with dementia and their carers. NICE guideline [NG97] [Internet]. 2018 [cited 14 February 2022]. Available from: https://www.nice.org.uk/guidance/ng97/
- https://www.bda.uk.com/resource/eating-and-drinking-difficulties-in-dementia.html
- Alzheimer’s disease: eating and drinking challenges. Gill Hooper. Network Health Digest. Vol 10.07. 16th July 2020
- Eating and drinking difficulties in dementia | British Dietetic Association (BDA)
- Eating and Drinking Well with Dementia – A Guide for Care Staff, Ageing and Dementia Research Centre, Bournemouth University 2018
- Volkert, Dorothee, Michael Chourdakis, Gerd Faxen-Irving, Thomas Frühwald, Francesco Landi, Merja H. Suominen, Maurits Vandewoude, Rainer Wirth, and Stéphane M. Schneider. "ESPEN guidelines on nutrition in dementia." Clinical nutrition 34, no. 6 (2015): 1052-1073.
- National Institute for Health and Care Excellence. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition NICE guideline [CG32] [Internet] 2006 [cited 14 February 2022]. Available from: nice.org.uk/guidance/cg32
- https://www.alzheimers.org.uk/sites/default/files/2019-09/448lp-dental-care-and-oral-health-190521.pdf
