A NUTRIENT-DENSE DIET TO OPTIMISE MUSCLE HEALTH IN OLDER ADULTS by Dove Yu, RD
Posted on
Malnutrition Awareness Week UK took place between the 10th and 16th October and raised awareness of the prevalence, signs, symptoms and consequences of malnutrition in older age.1 The BDA Older People Specialist Group focused on talking about muscle health and nutrition, given the increasing prevalence of sarcopenia in older adults. This blog will explain what sarcopenia is and how older adults can eat well to optimise muscle health.
WHAT IS SARCOPENIA?
Sarcopenia is a muscle disease rooted in adverse muscle changes that accrue across a lifetime (see Figure 1).2 It is common in older age but can also occur in earlier life. It reduces mobility, diminishes quality of life and increases the risk of falls and fractures, which require costly hospitalisation and extended rehabilitation.
In 2018, the European Working Group on Sarcopenia in Older People (EWGSOP2) updated the definition of sarcopenia. Overtaking the role of low muscle mass as a principal determinant of sarcopenia, the guideline identifies muscle strength as the key characteristic of sarcopenia with low muscle strength leading to a diagnosis of probable sarcopenia. Subsequent identification of low muscle mass in individuals who have low muscle strength is used to confirm its presence and, when physical performance is also poor, its severity (see Table 1).
Figure 1: Muscle strength throughout the life course2
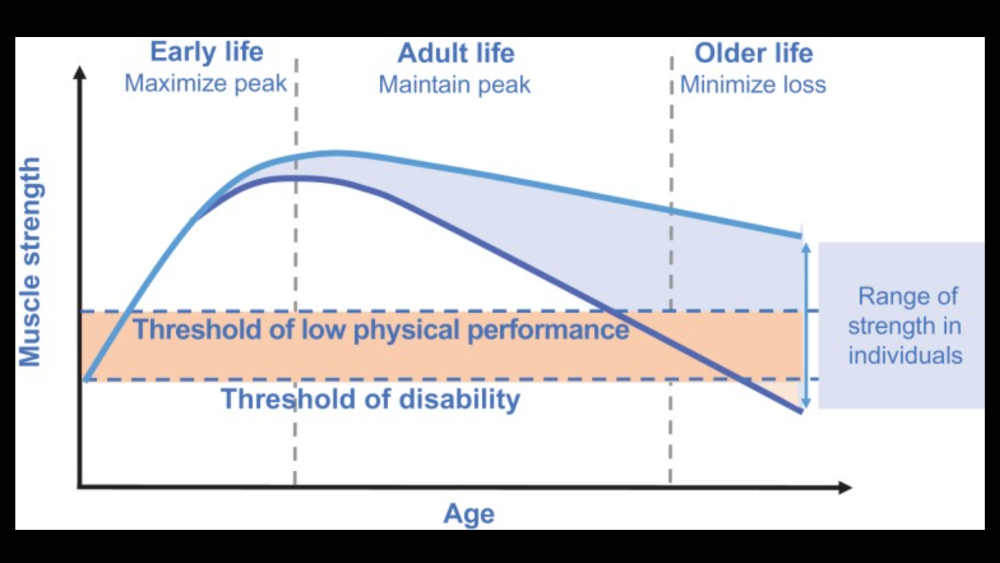
Table 1: 2018 operational definition of sarcopenia2
|
CRITERIA |
SARCOPENIA DIAGNOSIS |
|
1 Low Muscle strength
|
Probable sarcopenia is identified by Criterion 1.
|
|
2 Low muscle quantity or quality |
Diagnosis is confirmed by additional documentation of Criterion 2.
|
|
3 Low physical performance
|
If Criteria 1, 2 and 3 are all met, sarcopenia is considered severe. |
The Malnutrition Universal Screening Tool (‘MUST’) is widely used in clinical practice to indicate the need for nutrition support intervention, but the anthropometric measures, such as weight, BMI and weight loss, do not provide us with muscle strength, muscle quantity or quality and physical performance status. EWGSOP2 recommends use of the SARC-F questionnaire to identify probable sarcopenic patients.2 It is a self-reported questionnaire based on the individual’s perception of limitations in strength, walking ability, rising from a chair, stair climbing and falls. Practically, it is possible to measure muscle strength (eg, handgrip strength and chair stand test), muscle quantity or quality (eg, DXA, BIA, CT, MRI) and physical performance (eg, Gait speed, 400m walk).
A NUTRIENT-DENSE DIET TO OPTIMISE MUSCLE HEALTH
The link between nutrition and muscle health has been increasingly researched in recent years.3 A nutrient-dense diet that contains a balanced intake of all nutrients is important to optimise muscle health. It can be achieved by eating a variety of foods from different food groups, including protein, carbohydrates, dairy foods or alternatives and fruit and vegetables. Adequate hydration is also important to support normal muscle function.
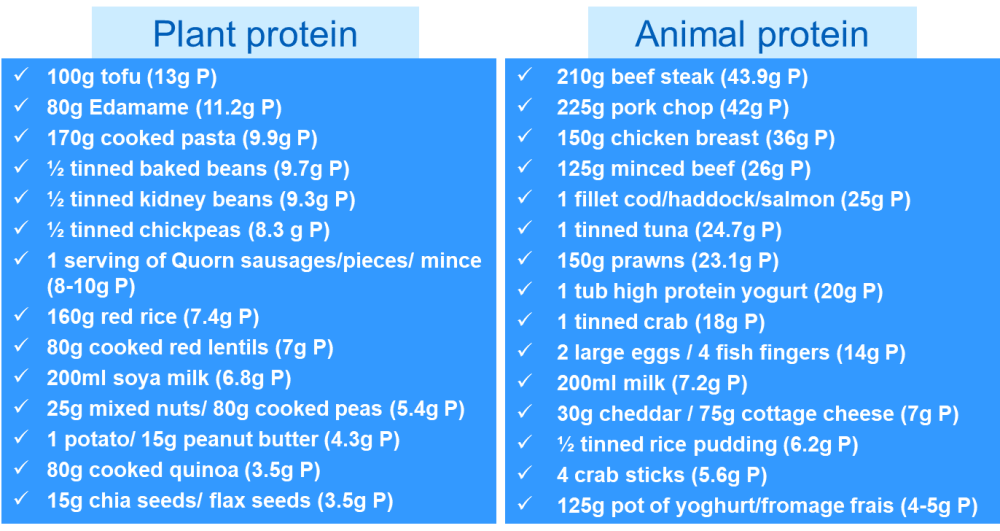
Multiple studies highlight the importance of 20-30g of high-quality protein evenly distributed at each meal to optimise protein synthesis in older adults.4-8 However, the exact amount remains controversial. The PROT-AGE study group9 has made recommendations on daily protein requirements in older adults, which are in line with EWGSOP2 and ESPEN recommendations10 (see Table 2). Figure 2 shows some of the examples of high-protein plant and animal foods.
Table 2: Daily protein requirements in older adults
|
|
DAILY PROTEIN REQUIREMENTS |
DAILY PROTEIN REQUIREMENTS BASED ON AN AVERAGE BODY WEIGHT OF A MALE AND FEMALE |
|
|
70kg male |
55kg female |
||
|
Healthy older people |
1.0-1.2g/kg |
70-84g |
55-66g |
|
Older people who are malnourished or have an acute/chronic condition |
1.2-1.5g/kg |
84-105g |
66-83g |
|
Those with severe illness/injury |
>1.5g/kg |
>105g |
>83g |
Figure 2: Protein contents in plant and animal foods
NICE CG32 emphasises that the overall nutrient intake of oral nutrition support offered should contain a balanced mixture of nutrients but not just calories.11 For those who are losing weight or underweight, food fortification should use more nutrient-dense ingredients, such as skimmed milk powder, cheese, egg, or nut spread, instead of just calorie-dense ingredients, such as cream, butter, or sugar. Snacks should also include more nutrient-dense choices, such as cheese and crackers, nuts, nut butter on bread, rice pudding with added skimmed milk powder, and thick and creamy yoghurt with fruit.
Nourishing drinks, such as Ovaltine, Horlicks and shop-bought vitamin-fortified milkshakes, can be made up with additional skimmed-milk powder and full-fat milk for a more nutritionally complete choice. For those who are overweight and obese, food and drinks that are lower in energy, fat and sugar but high in protein should be chosen. Examples of lean protein used in main meals include chicken breast, tinned tuna, or 5% fat lean mince. Examples of lower-calorie high-protein snacks include higher-protein yoghurt, soya yoghurt alternative, low-fat rice pudding, low-fat custard, and boiled eggs.
CONCLUSION
Loss of muscle strength and muscle mass is a natural part of ageing. A nutrient-dense diet is important to support muscle health. Nutrition and exercise are used as effective countermeasures for combating sarcopenia. Therefore, it is important that we keep moving. The BDA Older People Specialist Group has produced and shared a variety of graphics including tips and recipes to optimise muscle health. Feel free to follow us on twitter, Instagram and Facebook @bda_olderpeople.
Dove Yu RD, ANutr
Senior Specialist Dietitian (Nutrition Support/Palliative Care),
South Tees Hospitals NHS Foundation Trust.
Dove is PR Officer at BDA Older People Specialist Group
@BDA_olderpeople. She is passionate about person-centred care,
nutrition education and research, with experience in nutrition support
in both acute and community settings. Dove is interested in
food art and different food cultures.
Twitter@: doveyu_RD
Instagram: doveyu_dietitian
References
- Malnutrition Task Force (2022). UK Malnutrition Awareness Week 2022. Available from: https://www.malnutritiontaskforce.org.uk/uk-malnutrition-awareness-week-2022 [Accessed 10th Oct 2022]
- Cruz-Jentoft AJ et al (2018). Sarcopenia: Revised European consensus on definition and diagnosis, Age and Ageing, 48(1), p 16-31. Available from: https://doi.org/10.1093/ageing/afy169
- Robinson S, Granic A and Sayer AA (2019). Nutrition and muscle strength, as the key component of sarcopenia: An overview of current evidence. Nutrients, 11(12), p 2942. Available from: https://doi.org/10.3390/nu11122942
- Paddon-Jones D, Leidy H (2014). Dietary protein and muscle in older persons. Curr Opin Clin Nutr Metab Care, 17, p 5-11
- Deutz NE, Wolfe RR (2013). Is there a maximal anabolic response to protein intake with a meal? Clin Nutr, 32, p 309-313
- Mamerow MM et al (2014). Dietary protein distribution positively influences 24-hour muscle protein synthesis in healthy adults. J Nutr, 144(6), p 876-880
- Luiking YC, Deutz NE, Memelink RG et al (2014). Postprandial muscle protein synthesis is higher after a high whey protein, leucine-enriched supplement than after a dairy-like product in healthy older people: a randomised controlled trial. Nutr J, 13, p 9
- Thalacker-Mercer AE, Drummond MJ. The importance of dietary protein for muscle health in inactive hospitalised older adults. Ann N Y Acad Sci 2014, 1328, p 1-9
- Bauer J et al (2013). Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc, 14(8), p 542-59
- Deutz NE et al (2014). Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group Clin Nutr, 33(6), p 929-936
- NICE. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition NICE guideline [CG32] [Internet]. 2006 [cited 29 March 2021]. Available from: https://nice.org.uk/guidance/cg32 [Accessed 17th Oct 2022]
